We’re all familiar now with the parallels between our own pandemic moment and the international (“Spanish”) flu that ravaged the world just over a hundred years ago. The spread of masking (and anti-masking sentiment); moving classrooms outside; and other interventions during the Spanish flu serve as eerie echoes of our own pandemic policies. And the roaring `20s giving us a glimmer of hope that we, too, will come out of this crisis with a bright future.
But there another pandemic with lessons for the modern day. That’s the Russian flu pandemic of 1889-1890, which John Horton passes along. Recent speculation suggests that this pandemic was actually a new coronavirus affecting the human population; one of the four coronaviruses that now circulate in the population (OC43).
The story of this pandemic is fascinating — starting from Bukhara in Central Asia, it snaked along transcontininental train lines and steamers to steadily impact the whole world. Just like how boats spread the Plague of Justinian, trade caravans spread the bubonic plague, and planes have seeded our own pandemic—you see the vectors of spread of each pandemic reflecting in the dominant modes of transport.
And like the coronavirus we are now dealing with, the Russian flu primarily affected the elderly. It seems likely that pandemic wound up infecting a large fraction, if not a majority, of the world’s population; and killed maybe a million people. It even left chronic conditions among people who recovered, akin to long Covid.
Today, we are generally infected with these coronaviruses as children and they show up with cold-like symptoms. But that doesn’t mean they are harmless — an outbreak of OC43 led to the deaths of eight out of 95 infected residents in this nursing home, for instance. We just build immunity to these coronaviruses as children, generally avoiding worse outcomes later in life.
This now seems a plausible future for our current coronavirus pandemic as well.
How we Got to an Endemic Disease
At one point, there was a lot of hope that we could reach tangible herd immunity thresholds which would actually be enough to eradicate the Covid.
Maybe it was all wishful thinking at the time. But the math was reasonable and founded on the unusual effectiveness of the mRNA vaccines against the pandemic. The logic is that if you have an R0 of standard Covid of ~2-3, and mRNA vaccines are ~95% effective, you can calculate the herd immunity threshold as:
Herd Immunity = (1 / vaccine effectiveness) x (1 - 1/R0) = ~50-70%.
Now, if you take into account the fact that a good number of people have already been infected as well, and so have some natural immunity — you might need a little less than 70% of the population vaccinated to aim for close to eradication. So even with a small anti-vaxxer contingent; that seemed pretty reasonable goal to aim for.
This thesis started to change, and this was noted in real time, in January with the alpha variant in the UK. Increase R0 to a number more like 5, and the herd immunity number starts to shift into the high 80s. That gets a lot more dicey — but as long as vaccine effectiveness remains higher than that number (and the initial estimates really did suggest the vaccines remained quite effective against symptomatic Alpha) you can still think about eradication.
The Delta with Delta
Relative to that, Delta has had two main impacts. First, the R0 has shifted to a range more like 5-9, as the CDC guidance suggests.
But note that *if* the mRNA vaccines had the same efficacy, things could still be manageable. Herd immunity starts to be difficult with vaccination alone. But we still reach herd immunity at:
Percent Infected = (1 - 1/R0) - (efficacy vaccine x proportion vaccinated)
Which would be something like 33% at current vaccination rates. Youyang Gu has estimated that 29% of Americans were cumulatively infected through February; add in the infections since and we are plausibly over that number.
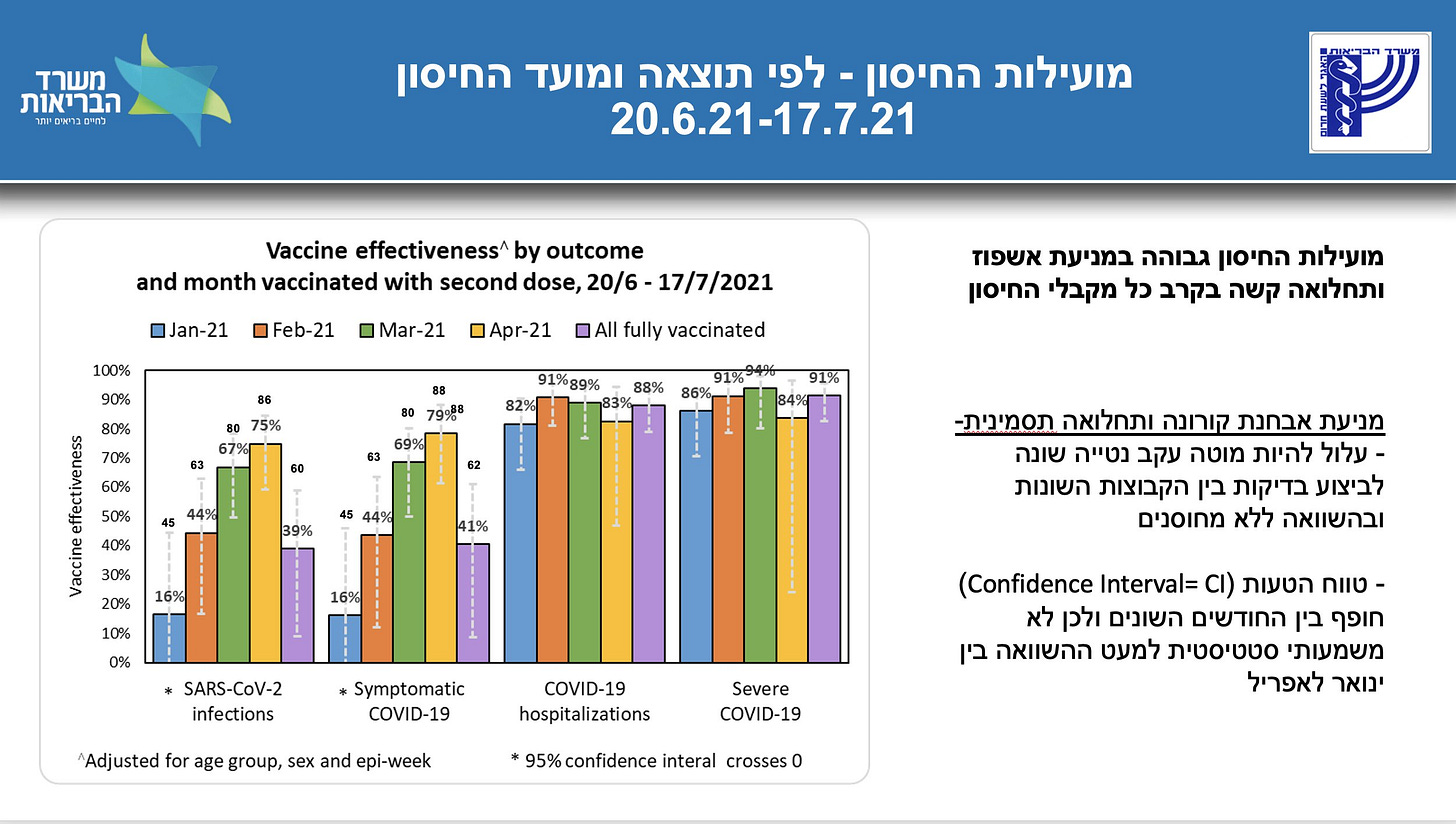
What really changes the picture is some combination of lower vaccine effectiveness against Delta and vaccines waning. Israel was the first sign of this: some preliminary estimates suggested that vaccine effectiveness might be 39% overall against Delta, and just 16% among those vaccinated the furthest back in time.
Now, the selection problems get really tricky here — the vaccinated and non-vaccinated groups are not assigned randomly, and there may be other differences in the behavior of these groups. In particular, it seemed like the initial Delta wave in Israel just happened to hit more vaccinated cities, making it hard to think about the right counterfactual comparison.
But we have good high-quality data on this question from the RAPID trial in the UK; which uses random sampling of testing across the population to gauge vaccine effectiveness. And they estimate vaccine effectiveness against symptomatic Covid of just 59% (averaged across AZ and Pfizer). They have a linked subsample of participants measured in successive waves, which seems to really suggest waning vaccines play a role.
What’s also neat is they can measure viral loads as an indicator of transmission — these do seem to be lower among the vaccinated. This is a little in tension with the Provincetown results which seemed to suggest the vaccinated are equally contagious. Again I think that speaks to the benefit of random sampling, rather than selecting the contagiousness of a subsample of vaccinated individuals sick enough to measure.
Anyway the point is that once you incorporate an effectiveness number like 59% (or 49% effectiveness against any infection at all); you start to get herd immunity numbers like 50-60% of Americans infected with covid at current vaccination rates. With presumably a lot of variation across heavily vaccinated and less vaccinated areas.
Now, it has to be emphasized that vaccines are still effective against hospitalizations and deaths, even over time, so this is all still a very optimistic scenario relative to a year ago. Still, it’s a pessimistic outcome relative to prevailing thought as of January this year.
Nothing is certain, but these numbers make it much more likely that covid becomes endemic. A sort of thing that stays with us; mostly causes the cold; and primarily affects new generations. We may need regular boosters. And it may occasionally hit clusters of vulnerable old people.
What Does This Mean For Policy?
First, we need to get vaccination rates as high as possible. It’s unclear how much would be “enough.” We’ve seen that even the most vaccinated country in the world — Malta — suffered a Delta wave. But the more vaccinations we can get, the fewer natural infections we have to deal with. So after moral persuasion and carrots in the form of lotteries — we are now moving more directly to mandates imposed by the local and federal governments on employees; and by private Universities and employers.
Second, the rationale for future NPIs needs to be carefully considered. I can sympathize with a locality that has low current vaccination rates pushing for temporary masking and other restrictions in the interim while they try to raise vaccination rates.
But what is the future for institutions like Universities that are fully vaccinated? The usual logic of flattening the curve — restricting mobility to shift cases in the future when we have a vaccine and are not overloading the hospital system — doesn’t really apply when we have no future improvements. A natural view here is what Sylvain Catherine suggests — institutions facing such environments should simply return to normal.

The biggest point of pushback here, I think, is the remaining risk of long Covid, even among vaccinated individuals. I think that’s a topic we simply don’t know enough about yet.
But I want to argue there is one other big thing we should shift our policy focus to — ventilation.
Ventilation
There was a really fascinating story in WIRED about the nature of Covid that didn’t get enough attention. This is a really detailed story that argues scientists made two critical errors in assessing the transmissibility of respiratory diseases. First, they took for granted a 5 micron limit as defining the threshold for airborne spread. Second, they assumed that other airborne diseases like measles must have very high contagiousness; reinforcing the idea that non-hyper contagious diseases are not airborne.
The upshot is that we were locked into a bad paradigm for the spread of respiratory diseases this whole time. It was assumed that colds and flus spread primarily through droplets — heavier particles which directly hit close by individuals, and may spread through contact on surfaces (fomites). Aerosol spread — which could be contained instead through masks and ventilation — was ruled out as a source of spread for these diseases in general.
Now, we have good data to suggest that SARS-CoV-2 spreads predominately through airborne transmission. But the initial failure to pick this up was an error with pretty massive consequences, akin to simply not understanding how cholera spread until John Snow’s experiments or sticking to the “miasma” theory which was common back in the Russian flu (In fact, there is an idea that doctors over-corrected from the bad miasma theory to be routinely skeptical of aerosol spread in general).
The misdiagnosis led directly to initial efforts to downplay masks; and to instead focus on social distancing, hand washing, and surface cleaning as our key strategies. But this simply follows the playbook for respiratory diseases in the past — it seems likely that we have simply undervalued the importance of masks and ventilation as valuable methods of disease reduction for colds and flus in general; not just with covid.
Masks are of course helpful; and people should be encouraged to wear them as needed even after the pandemic is over — especially for riskier populations and people experiencing cold symptoms. But it’s probably not realistic to expect people to mask as often as they have for the last few months.
And this is why understanding the central role for aerosols in driving the spread of this generic family of respiratory illnesses means focusing on indoor ventilation.
Better ventilation and airflow can basically lower the concentration of contagious particles in indoor spaces without requiring any active action by people. And, as we have historically built up our physical environment, we simply have not taken into account enough the fact that better ventilation also improves our health; and can lower the rate of sickness and productivity-draining illnesses. Internalizing these health benefits calls for an upgrade of our entire country’s ventilation systems.
Industrial Policy for Ventilation
So this is my tangible proposal — we systematically invest in ventilation across the nation’s schools, workplaces, retail stores, and other indoor spaces. Covid may ultimately become one of several low-grade respiratory diseases in the population: but why not lower the R on all of these diseases, simultaneously, by directly lowering the rate at which they spread?
To do this, I would suggest a key financing role can be played by Fannie and Freddie. These institutions already have a Green Bond program which offers loans to multifamily properties intended to retrofit the existing housing stock to be more energy and water efficient. In fact the loans record changes in tangible environmental metrics for end investors.
I think Fannie and Freddie could open up similar lending facilities to commercial real estate across the board, intended to directly finance investments in improved ventilation. In tandem, the CDC could steadily improve guidance on ventilation standards and best practices so firms know what’s expected.
Normally, I’d be all about some sort of value capture here — but unlike improvements in water or energy efficiency; savings from improved health that result in fewer children and employees getting sick are probably hard to measure. So I’d be fine with trying to to nudge our existing real estate stock in a more healthy direction through federal means. This would be sort an industrial policy program, leveraging our federal control over these mortgage giants, to achieve a boost to our public health infrastructure. And just like we responded to the threat of cholera (once properly understood) by improving the water supply; we can address coronavirus by fixing our air.
We need to adapt to a world in which we simply face some endemic disease risk, and we need to have a debate on how to move the tangible levers we have — including ventilation.
Update: There is a nice piece here at Science on Joseph Allen, who has been advocating for better air quality even before the pandemic. It includes some interesting data here on the broader productivity implications of circulation:
In a multiyear series of experiments, Allen and his team have investigated the consequences. In the first study, published in 2015, they had 24 white-collar volunteers spend six working days in environmentally controlled office spaces at Syracuse University's Total Indoor Environmental Quality Laboratory. On various days the experimenters would alter ventilation rates and levels of CO2 and VOCs. Each afternoon the volunteers were tested on their ability to think analytically and react to a crisis. (One test, for example put the volunteer in the role of a small-town mayor trying to react to an emergency.) All tests were double-blind: Neither the volunteers nor the study personnel knew that day's environmental conditions.
The results were dramatic. When volunteers worked in well-ventilated conditions (which lowered the levels of CO2 and VOCs), they scored 61% higher than when they worked in typical office building conditions. When they worked in the cleanest conditions, with even lower CO2 levels and higher ventilation rates, their scores climbed 101%.
To find out whether the results held up in the real world, Allen and his team recruited 109 volunteers from 10 office buildings across the United States. Six had been renovated to create better heat and humidity control, improve ventilation, and lower the use of toxic materials. Four had not. Allen's team gave each office worker a Fitbit-like bracelet to record heart rate, skin temperature, sleep patterns, and other physiological signs of well-being. Workers also completed a survey each day about how comfortable they felt and whether they experienced symptoms such as drowsiness or headaches. At the end of the week, they took the cognitive tests. Workers in the buildings with good ventilation and lower levels of indoor pollution scored 26.4% higher than those in the unimproved buildings. They also reported sleeping better and experiencing fewer “sick building” symptoms.